Patient Assessment
The following program will inform you of the best possible ways you can assess your patient. We will go over what Patient Assessment is as well as cover a variety of assessments.
What is patient assessment?
“Patient Assessment is the process used to identify and treat life-threatening problems, Assessment concentrating on Level of Consciousness, Cervical Spinal Stabilization, Airway, Breathing, and Circulation.” - NY State Department of Health
There are multiple types of Patient Assessment used in many different scenarios, and these are used to gain as much information about the patient as possible to perform the best treatments for the situation.
Primary Assessment
Primary Assessment or Initial Assessment is a rapid, initial examination of a patient to recognize and manage all immediate life-threatening conditions.
Determine Responsiveness - Can you get a response from the patient? Is the patient conscious? Do they respond to you when you talk to them, touch their hands or squeeze their shoulder? (AVPU)
(X) External Bleeding - Is the patient bleeding? If so pack the wound with gauze and apply a tourniquet if needed/possible.
(A) Airway - Are the patient’s nose and throat clear? Check for any foreign material such as blood, vomit, etc. If present, roll the patient onto their side and remove the material. Remember, Life over Limb. If needed you can move someone with a suspected spinal injury to clear the airway.
(B) Breathing - Is your patient breathing on their own? Look for the rise and fall of the chest. Listen for breathing sounds. Feel for inflation and deflation of the lungs.
(C) Circulation - Does your patient have a pulse? If not, start performing CPR. If they do, start to provide basic treatment for any injuries found.
Pain Assessment
Pain assessment is always an ongoing process rather than a single event, as the patient’s level of pain may change drastically depending on the situation. If you think your patient is in pain, you should use the Mnemonic OPQRST (Onset, Provocation, Quality, Radiation, Severity, Time).
Onset - When did the pain Start? What were you doing when it started?
Provocation - Does anything calm the pain or make it worse?
Quality - What does the pain feel like? Describe what you feel.
Radiation - Does pain go anywhere? If so, where?
Severity - Rate your pain on a scale of 1 to 10, 1 being the least severe and 10 being the most severe.
Time - How long has the pain been going on?
If the patient’s vital signs change drastically and the patient seems to be in pain, act accordingly.
Illness Assessment
Illness assessment is much harder to diagnose and assess than would appear, due to the multitude of possibilities. The best way to determine what may be affecting the patient is to look at their symptoms and cross out any possible causes. If you believe the patient is afflicted with an illness, use the SAMPLE (Signs/Symptoms, Allergies, Medications, Pertinent Medical History, Last Oral intake, Events leading up to) mnemonic to aid with diagnosis.
Signs/Symptoms - How are you feeling? Why did you call 911?
Allergies - Do you have any allergies?
Medications - Do you take any medications? Were there any recent changes to the medications you take?
Pertinent Medical History - Any health problems in the past that made you go to the hospital for?
Last Oral Intake - What was the last thing you ate and drank?
Events Leading Up To - What were you doing before and in the moment where this first started?
Always prioritize maintaining patient vitals and keeping the patient stable. If any of the patient’s vitals seem to deteriorate, act accordingly.
Medical History
“The purpose of obtaining a health history is to gather subjective data from the patient and/or the patient’s family so that the health care team and the patient can collaboratively create a plan that will promote health, address acute health problems, and minimize chronic health conditions.” - “Clinical Procedures for Safer Patient Care” by Glynda Rees Doyle
When determining past and current medical history you should follow this checklist to ensure you don’t forget anything pertinent to an eventual diagnosis.
Medical History Checklist:
- Information about the patient (Name, Age, Occupation, Marital Status)
- Reason for Seeking care and history of present health concern (Use OPQRST and SAMPLE Mnemonics to aid with this)
- Past Medical history (Allergies, Serious illnesses, Recent hospitalizations and surgical procedures, Emotional or psychiatric problem (if still pertinent), current medications, Drug/Alcohol consumption.)
- Family Medical history
- Functional assessment (Does patient exercise? Eat healthy? Sleep/rest adequately etc.)
Trauma Assessment
There are many different levels of severity to trauma patients. Some could just have scrapes and small lacerations while others could have a Traumatic Brain Injury which is much more severe, for example. When doing your primary assessment, if a MOI or Mechanism of Injury is known, look for injuries relative to that specific MOI. If trauma is severe or Mechanism of Injury is unknown, perform a full trauma assessment explained in the next slide.
Once you have completed your assessment, treat the patient accordingly.
Full Trauma Assessment
There are many different levels of severity to trauma patients. Some could just have scrapes and small lacerations while others could have a Traumatic Brain Injury which is much more severe, for example. To determine the severity of each individual patient we follow a specific mnemonic. DCAP-BTLS.
D - Deformities (Any deformations on the patient’s body?)
C - Contusions (Any bruises on the patient’s body?)
A - Abrasions (Any abrasions?)
P - Penetration (Is there anything penetrating the patient?)
B - Burns (Are there any burns to the patient? If so how severe?)
T - Tenderness (Does the patient appear to be in pain when you touch a specific area? If so, where?)
L - Lacerations (Are there any lacerations on the patient’s body?)
S - Swelling (Is there any swelling on the patient’s body?)
The answers to the questions above will then determine the severity of the trauma patient. Once the assessment is complete, please treat the patient accordingly.
Lung Sounds
There are multiple types of abnormal lung sounds, each caused by different reasons. When you are listening to lung sounds you want to look for a continuous, bilateral, low pitched breathing noise. Anything other than this is regarded to be abnormal.
Skin Color and Condition
Skin condition and color is an easy way of determining if the patient is able to oxygenate themselves efficiently and provide oxygenated blood to their tissues.
Color:
For the lighter skin color patients you will find their skin to have a pink color or tone when receiving adequate blood flow, and a paler look otherwise. For the darker skinned individuals you may need to check the palms of the patient’s hands or the mucous membranes in their mouth.
Condition:
Skin condition typically falls under the following categories: normal, dry, moist, or diaphoretic. Patients with diaphoretic skin will appear to be sweating profusely and it is associated with many conditions, notably heart conditions, hypoglycemia, shock and alcoholism.
Temperature:
Skin temperature is typically warm. A hot temperature can indicate fever, exposure to heat with possible hyperthermia or infection. A cool temperature may indicate Shock, inadequate circulation or exposure to cold. A cold temperature indicates extreme exposure to the cold with possible hypothermia.
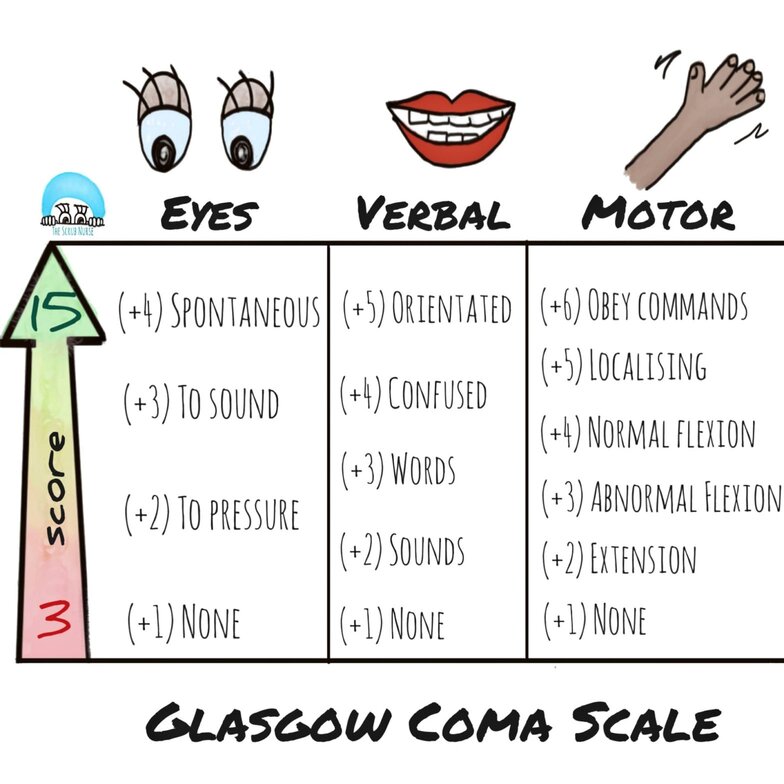
Glasgow Coma Scale
“The Glasgow Coma Scale was designed and should be used to assess the depth and duration coma and impaired consciousness. This scale helps to gauge the impact of a wide variety of conditions such as acute brain damage due to traumatic and/or vascular injuries or infections, metabolic disorders.” - CDC
To determine someone’s GCS score, follow this list of points.
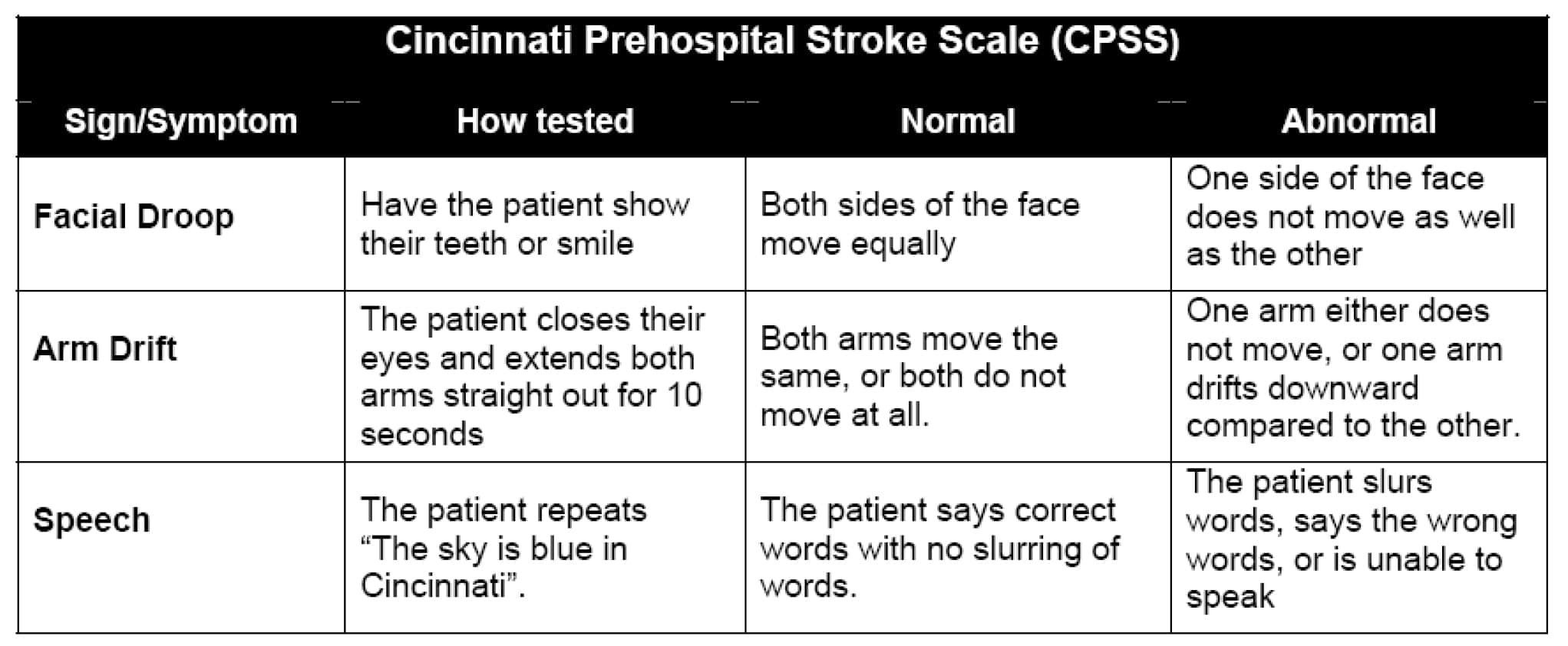
Cincinnati Stroke Scale
The Cincinnati stroke scale was designed to diagnose a potential stroke in a prehospital setting. It tests for 3 signs of a stroke. If any of these signs are visible, “the probability of a stroke is 72%”. - American Stroke Association
Facial Droop
Have patient smile.
- Normal: Both sides move equally
- Abnormal: One side does not move as well as the other.
Arm Drift
Have your patient close their eyes and extend their arms, palms up for 10 seconds
- Normal: Both arms move the same or not at all
- Abnormal: One arm does not move or drifts down relative to the other
Abnormal Speech
Have your patient say “you can’t teach an old dog new tricks”
- Normal: Patient uses correct words without slurring
- Abnormal: Patient slurs words, uses the wrong words or is unable to speak
Pupils during patient assessment
Pupil response is an essential part of a provider’s patient assessment. The patient’s pupil diameter and the way they respond to light can give you an idea of what the status of the brain is. To assess a patient’s pupils, we use the mnemonic PEARRL.
- P - Pupils
- E - Equal
- A - And
- R - Round
- R - Regular in Size
- L - Light / Reacts to Light
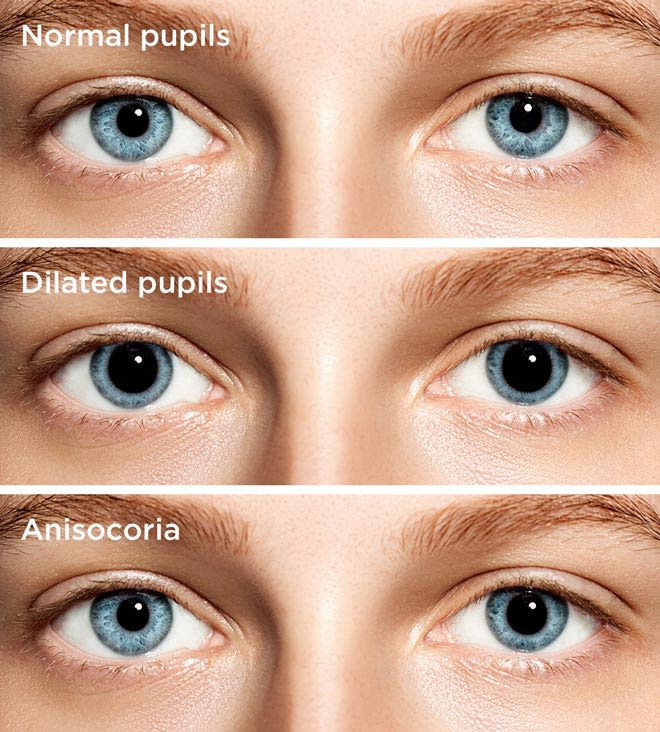
After patient assessment is complete, you should report your findings. If the patient has normal pupils, you should report “The patient’s pupils are PEARRL”.
If you encounter something abnormal, such as the image above, you should report “The patient’s left pupil is regular in size and reacts to light, the patient’s right pupil is fixed and dilated.”
Vital Signs (Adult)
These are the vital signs for the average adult. Anything higher or lower than these vital signs could be life threatening and should be treated accordingly.
Note: An Athletic adult could have a lower resting heart rate than the one listed below, for example.
| Body Temperature | 98.6ºF (36.5ºC) |
| Heart Rate | 60-100 BPM (Beats per minute) |
| Respiratory Rate | 12-22 BPM (Breaths per minute) |
| Blood Pressure | 120/80 (Textbook perfect, can vary) |
| Blood Glucose Level (BGL) | 80-100 BGL |
Mnemonics
SAMPLE:
- S - Signs/Symptoms
- A - Allergies
- M - Medications
- P - Pertinent Medical History
- L - Last Oral Intake
- E - Events Leading Up To
OPQRST:
- O - Onset
- P - Provocation
- Q - Quality
- R - Radiation
- S - Severity
- T - Time
AVPU:
- A - Alert
- V - Verbal
- P - Painful
- U - Unresponsive
DCAP-BTLS
- D - Deformities
- C - Contusions
- A - Abrasions
- P - Penetration
- B - Burns
- T - Tenderness
- L - Laceration
- S - Swelling
XABC
- X - External Bleeding
- A - Airway
- B - Breathing
- C - Circulation